RPM Billing 2025: CMS Compliance & Practical Solutions

Implementing the new CMS guidelines for Remote Patient Monitoring (RPM) billing in 2025 requires healthcare providers to adopt practical solutions for seamless compliance and effective patient care.
As healthcare continues its rapid evolution, particularly accelerated by technological advancements, understanding and adapting to regulatory changes is paramount. This guide provides practical solutions: implementing the new CMS guidelines for Remote Patient Monitoring billing – a step-by-step guide for 2025 compliance, ensuring your practice is not only compliant but also optimized for the future of digital health.
Understanding the 2025 CMS RPM Landscape
The Centers for Medicare & Medicaid Services (CMS) continually updates its guidelines to reflect the dynamic nature of healthcare delivery, especially in the realm of remote patient monitoring (RPM). For 2025, these updates bring both opportunities and challenges, requiring a deep dive into the nuances of billing codes, documentation requirements, and patient eligibility criteria.
Navigating this landscape effectively means understanding the ‘why’ behind these changes. CMS aims to enhance patient outcomes, improve access to care, and reduce healthcare costs through the strategic use of remote technologies. Providers must align their operational strategies with these overarching goals to maximize the benefits of RPM.
Key Changes and Their Impact
The 2025 CMS guidelines introduce several modifications that will directly impact how healthcare practices implement and bill for RPM services. These changes often focus on refining service definitions, clarifying eligible providers, and specifying minimum data collection requirements.
- Expanded Eligibility: CMS might broaden the scope of conditions or patient populations eligible for RPM, increasing the potential reach for providers.
- Refined Service Codes: New or revised CPT codes could be introduced, necessitating a thorough review of existing billing practices.
- Documentation Standards: Stricter requirements for documenting patient consent, device use, and clinical interventions are anticipated.
- Data Transmission & Review: Clearer rules on how data should be collected, transmitted, and reviewed by clinical staff will be emphasized.
These adjustments underscore the importance of proactive preparation. Practices that embrace these changes early will be better positioned to maintain compliance and leverage RPM as a core component of their care delivery model. Understanding the foundational elements of these updates is the first step toward successful implementation.
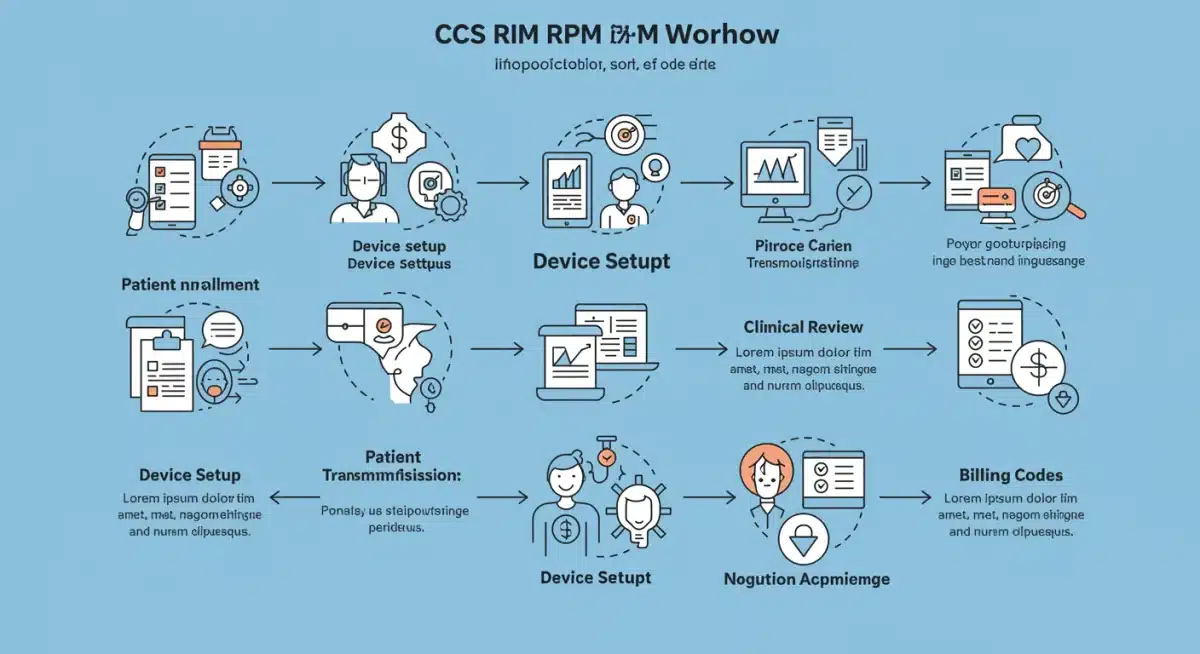
Step-by-Step Guide to 2025 CMS RPM Compliance
Achieving compliance with the 2025 CMS guidelines for RPM billing requires a structured approach. This section outlines a step-by-step methodology to ensure your practice seamlessly integrates the new requirements and maintains a high standard of care.
From initial assessment to ongoing monitoring, each phase plays a critical role in establishing a robust RPM program. The goal is not just to meet the minimum standards but to build a sustainable and effective system that benefits both patients and providers.
Phase 1: Assessment and Planning
Begin by conducting a comprehensive internal assessment of your current RPM capabilities and existing billing processes. Identify any gaps between your current practices and the anticipated 2025 CMS guidelines. This phase involves reviewing your patient demographics, technology infrastructure, and staffing models.
- Review Current Practices: Document existing RPM workflows, devices used, and patient onboarding procedures.
- Identify Gaps: Pinpoint areas where your practice falls short of new CMS requirements, such as documentation, data frequency, or eligible conditions.
- Resource Allocation: Determine necessary resources, including personnel training, technology upgrades, and potential partnerships.
Developing a detailed action plan based on this assessment is crucial. This plan should outline specific tasks, responsible parties, timelines, and measurable outcomes. A well-defined plan ensures a smooth transition and minimizes disruptions to patient care.
Technology Integration and Device Selection for RPM
The success of any RPM program hinges significantly on the technology employed. Selecting the right devices and ensuring seamless integration with existing electronic health records (EHR) systems are critical steps for 2025 CMS compliance. The chosen technology must not only meet regulatory standards but also enhance patient engagement and clinical efficiency.
Consider the user-friendliness of devices for patients, the reliability of data transmission, and the security protocols in place. A robust technological infrastructure supports accurate data collection and facilitates timely clinical interventions, both essential for effective RPM.
Choosing Compliant Devices
When selecting RPM devices, prioritize those that are FDA-cleared and capable of capturing the specific physiological data required by CMS for billing purposes. Ensure devices are easy for patients to use at home, minimizing technical barriers to adherence.
- FDA Clearance: Verify that all chosen devices are FDA-cleared for their intended use, ensuring data accuracy and safety.
- Data Compatibility: Ensure devices can integrate with your EHR system to streamline data flow and reduce manual entry errors.
- Patient Usability: Select devices that are intuitive and require minimal technical expertise from patients, encouraging consistent use.
An effective device strategy involves a balance between technological sophistication and practical application in a home setting. Regular evaluation of device performance and patient feedback is also vital for continuous improvement and compliance.

Documentation and Billing Best Practices
Accurate and thorough documentation is the backbone of successful RPM billing and CMS compliance. The 2025 guidelines are expected to place an even greater emphasis on meticulous record-keeping to justify services rendered and ensure proper reimbursement. Implementing robust documentation practices is non-negotiable.
Every interaction, every data point, and every clinical decision related to RPM must be clearly recorded. This not only supports billing claims but also provides a comprehensive patient record, essential for coordinated care and legal protection.
Mastering CPT Codes and Modifiers
A deep understanding of the relevant CPT codes for RPM services is fundamental. For 2025, anticipate potential revisions or new codes that will require updated billing protocols. Pay close attention to the specific requirements associated with each code, such as minimum data collection days or interactive communication time.
- Code Review: Regularly review CMS updates for new or modified RPM CPT codes to ensure accurate billing.
- Time Tracking: Implement systems to accurately track time spent on RPM services, especially for codes requiring specific durations of clinical review or patient interaction.
- Modifier Application: Understand and correctly apply modifiers to CPT codes, as they can significantly impact reimbursement and compliance.
Proper documentation extends beyond just billing codes; it includes patient consent, device distribution records, and a clear summary of all RPM data reviews and subsequent clinical actions. Training staff on these best practices is crucial to avoid common billing errors and potential audits.
Staff Training and Patient Engagement Strategies
Even with the most advanced technology and robust compliance plans, the human element remains central to successful RPM implementation. Comprehensive staff training and effective patient engagement strategies are critical for optimizing the benefits of RPM and ensuring adherence to CMS guidelines for 2025.
A well-trained team can confidently navigate the technological aspects, interpret data, and provide meaningful care. Engaged patients are more likely to use their devices consistently, leading to richer data sets and improved health outcomes.
Empowering Your Team
Invest in thorough training programs for all staff involved in RPM, from administrative personnel handling enrollment and billing to clinical staff monitoring data and interacting with patients. Training should cover not only the technical aspects of RPM devices and software but also the clinical protocols and CMS documentation requirements.
- Technical Proficiency: Ensure staff are comfortable with device setup, troubleshooting, and data management within the RPM platform.
- Clinical Protocols: Train clinical staff on interpreting RPM data, identifying actionable insights, and intervening appropriately.
- Billing & Compliance: Educate administrative and billing staff on the latest CPT codes, modifiers, and documentation standards for 2025.
Beyond initial training, provide ongoing education and support to keep staff updated on any new CMS directives or technological advancements. Fostering a culture of continuous learning is paramount for long-term RPM success.
Monitoring, Auditing, and Continuous Improvement
Compliance with CMS guidelines for RPM billing is not a one-time event but an ongoing process. Establishing robust monitoring, internal auditing, and continuous improvement mechanisms is essential to adapt to evolving regulations and optimize your RPM program for 2025 and beyond.
Regularly assessing your RPM operations allows for early identification of potential issues, quick rectification, and the proactive implementation of enhancements. This proactive approach safeguards against compliance risks and ensures the sustained effectiveness of your remote care initiatives.
Implementing Internal Audit Processes
Develop and implement a schedule for regular internal audits of your RPM program. These audits should review all aspects, including patient enrollment, device distribution, data collection, clinical review, documentation, and billing practices. Use a checklist approach to ensure all CMS requirements are being met consistently.
- Data Integrity Checks: Verify the accuracy and completeness of data transmitted from RPM devices to your EHR.
- Documentation Review: Scrutinize patient consent forms, clinical notes, and billing records for compliance with CMS standards.
- Billing Code Verification: Confirm that CPT codes and modifiers are being applied correctly based on services rendered and documented.
Feedback from these audits should be used to identify areas for improvement, refine workflows, and provide targeted training to staff. A continuous improvement loop ensures that your RPM program remains agile, compliant, and highly effective in delivering quality patient care.
| Key Point | Brief Description |
|---|---|
| 2025 CMS Updates | New guidelines for RPM billing, emphasizing expanded eligibility and stricter documentation. |
| Technology Integration | Selecting FDA-cleared, EHR-compatible devices for accurate data collection and patient ease of use. |
| Documentation & Billing | Mastering CPT codes, modifiers, and meticulous record-keeping to ensure proper reimbursement. |
| Ongoing Compliance | Implementing continuous monitoring, internal audits, and staff training for sustained RPM program effectiveness. |
Frequently Asked Questions About 2025 CMS RPM Billing
The 2025 CMS RPM billing guidelines are expected to refine existing codes, potentially expand patient eligibility, and introduce stricter documentation requirements. These changes aim to improve the quality and accountability of remote patient monitoring services, ensuring better patient outcomes and more efficient healthcare delivery.
To ensure compliance, practices should implement detailed record-keeping systems for patient consent, device distribution, daily data collection, and all clinical interactions. Regular staff training on updated CMS requirements and internal audits of documentation practices are also crucial to maintain accurate and defensible records.
Technology is central to 2025 CMS RPM compliance. Practices must utilize FDA-cleared devices that seamlessly integrate with EHR systems. The technology should facilitate accurate data capture, secure transmission, and efficient clinical review, while also being user-friendly for patients to ensure consistent engagement and data flow.
Staff should receive initial comprehensive training when implementing new RPM guidelines, followed by regular refreshers. Ideally, training should occur whenever CMS releases significant updates, new CPT codes are introduced, or internal audit findings reveal areas for improvement. Continuous education ensures ongoing compliance and proficiency.
Proactive RPM compliance offers numerous benefits, including optimized reimbursement, reduced audit risks, and enhanced patient care. By staying ahead of regulatory changes, providers can efficiently leverage RPM to improve patient outcomes, expand access to care, and position their practice as a leader in digital health innovation.
Conclusion
The 2025 CMS guidelines for Remote Patient Monitoring billing represent a significant evolution in healthcare delivery, pushing practices towards more integrated and technologically advanced care models. By embracing a strategic, step-by-step approach to implementation, providers can not only ensure compliance but also unlock the full potential of RPM. This involves meticulous planning, careful technology selection, stringent documentation, comprehensive staff training, and a commitment to continuous improvement. Navigating these changes effectively will position healthcare organizations to provide high-quality, efficient, and compliant remote care, ultimately benefiting both patients and the financial health of the practice.





